Reframe pain and relief with new neuroscience and options.
"Pain is your brain’s opinion of how safe you are." For low back pain, this means more than muscle or disc issues—it’s also about how your brain interprets danger based on past experiences. Chronic back pain often lingers when fear and a lack of control turn up the volume. Learn how to turn it down. Explore multimodal options that address both body and brain, and build your own plan using science-backed strategies. Find support, tools, and the latest research on What Works for Low Back Pain.

A Brief Biology of Pain - Resources - Physiology, Movement, and Pain Relief - What Works for Pain
We know some pain is unavoidable. We know opioids can improve lives. And while we also know there is no one right answer for pain relief, by using new neuroscience and choosing multiple effective options, everyone can become more comfortable. While we founded the field of thermomechanical pain relief, we support every evidence-based pain intervention - and want you to know about them all. To understand why science supports reframing pain and that relief is attainable (with work), read on, or skip down to resources. (For deeper study, we highly recommend McGill University's interactive website The Brain.)
“What if pain isn’t an alarm we should silence, but a learning system for survival?” - Dr. Amy Baxter
Pain is an organism's most basic learning system. In order to learn from the sensations brought in from the body, pain passes through the filter of the spine, then through a filter in the brain, then a switchboard that connects to multiple brain processing areas. While these areas have different functions (memory, options, identity, fear, optimism, movement) what we feel as "pain" is the sum of all the areas connected to a sensation. These "connectomes" can become thick enough to feel pain even when the sensation wouldn't normally be painful... or isn't there anymore at all.
By overriding pain at the level of the spine filter, jamming the switchboard, strengthening connections that reduce pain, countering pain with incompatible brain patterns, and deconstructing the connections, both acute and chronic pain can become more comfortable, or manageable, or even resolve. Our modern lifestyles (and instant gratification culture!) don't help, but with practice and understanding WHY, options and reframing can give power over pain.
With pain that began from damage, the body has multiple ways to deconstruct the connections to reduce pain.
With pain that is ongoing from inflammation, or comes and goes from a genetic risk, understanding brain pathways can still get to "more comfortable". At Pain Care Labs, we deeply hope that breakthroughs in long COVID will lead to help for fibromyalgia, neuropathies, mast cell activation, and other inflammatory processes leading to chronic pain.
If you have other resources that have helped you, or you run an organization that helps, please reach out for inclusion.
Find a medical massage therapist
Massage therapy directly reduces pain, increases the neurotransmitters of serotonin and oxytocin that reduce pain, and can improve or prevent the pain after injury from smaller muscles trying to compensate, leading to more pain than the injury itself.
Find a Physical Therapist who specializes in pain
To find a physical therapist who specializes in pain, ask whether they have experience in myofascial release, dry needling, and pain evaluation.
Find a pain psychologist
Chronic pain can both come FROM genetically altered reward receptors and can contribute to ongoing depression, frustration, and altered relationships. Specialists get how isolating chronic pain and be and how to help.
Advocating in a crisis
This Health Central article by Dr. Baxter discusses ways to communicate chronic pain or illness to emergency physicians; the Invisible Project quotes Dr. Amy Baxter and others on how to be heard when you have a pain flare in the emergency department.
A national non-profit charitable organization that helps chronic illness, including pain, with financial assistance, advocacy, and awareness.
Rather than trying to find experts in multiple aspects of pain management, Override is a fee-based sliding scale or insurance-supported pain team aggregator. They coordinate virtual visits with you with a pain physician, a chronic pain-trained physical therapist, a pain psychologist, and a certified pain management coach who works individually with you and together as a team.
Prescriptions/year
Source of Misused Opioids
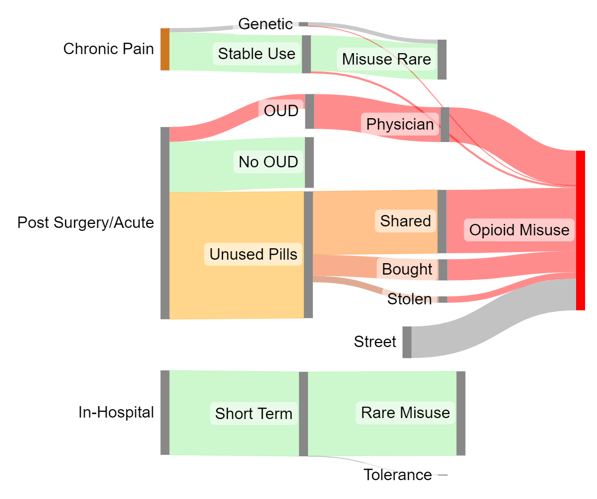
Lack of adequate pain relief options after surgery and with acute pain is a societal problem. Because so many people have leftover opioids available "just in case", fentanyl-laced imposters don't raise red flags. As shown in this graphic, almost all of these leftover opioids come after acute pain and surgery. If we had better options, preventing leftover pills would be easier.
Note: Not all of the curated list below are non-profit, but all are founded by people who have been personally impacted by pain and care about pain relief. While we only included sites with heavily evidence-based suggestions, Pain Care Labs does not endorse or take responsibility for all options on all sites, but provides these links as a resource.
Empathetic, evidence and personal experience based resources from an amazing woman "loving, living and learning with chronic pain, chronic fatigue and insomnia".
This free online health community has curated stories and lived experiences with advice, moderated 24/7 chat support, and tips and advice from other people with chronic pain, fibromyalgia, and more.
PainCommunity.org
This non-profit was started by advanced practice nurses with pain expertise to support a diverse community by promoting Comprehensive Integrative Pain Management (CIPM) education, wellness information, and advocacy for quality pain care.
US Pain Foundation
An organization created by and for the 51.6 million Americans in daily pain. They strive to be the leading support for those living with pain, caregivers, and care providers.
How can ice + vibration replace Oxycontin?
1 - Cold : Very cold sensations (cryotherapy) slow nerve conduction and pain signals, but also cause the brain to activate pain inhibition.
2 - Vibration: activating the Pacinian nerve with fast motion is the most effective gate control touch sensation, and can reduce pain directly, or when it's put "between the brain and the pain".
3 - Agency: a feeling of control (e.g. by choosing when to place VibraCool,) the physical activity of intervening, and optimizing the position of relief via biofeedback ("oh, that's a good spot) all reduce pain intensity
4 - Choice: actively deciding when and what to do about a problem engages the anterior cingulate cortex (switchboard), so pain connections are lessened and you feel less pain
5 - Options: the area of the brain that is more active in optimistic people is also the area that sorts through multiple options ...and the area that is least active with chronic pain. More top-of-mind options make it easier to SORT options, and feel empowered.
6 - Grit/Stubbornness/Goal Setting: The most crucial part of not taking or limiting opioids after surgery is simply the decision not to. An orthopedist accustomed to giving 50 Percocet after an ACL reconstruction found the athletes in his practice regularly took 25 and saved the rest. He decided to reduce the number prescribed to 30... and his patients then only took 15. No change in pain or satisfaction scores. The point is that opioids are a small part of home post-op pain management. The amount used isn't what is "needed", but what the physician and our culture telegraph is expected. In most other countries, what is "expected to be needed" is... none. Hence, ice and vibration can be part of a plan of distractions and interventions after acute pain to get through the rough first few days while the body heals, and can work just as well as depending on a mildly effective intervention with extraordinary risks.
How can ice + vibration help you get to sleep? (Question from YouTube answered by Dr. Baxter)
One of the great ironies is that medications that make one drowsy (opioids for some people, alcohol for others) cause disrupted and untherapeutic sleep (i.e. without restorative deep sleep). This is purely anecdotal here, but I've had lots of pain events and accidents, and I have a sleep-tracking ring so I can see after the fact what happens with my sleep. When I've been awoken by screaming pain in my shoulder after multiple rotator cuff tears, when there's spasm, the heat and vibration reduce pain enough that I can relax - and almost instantly go to deep sleep. When it's just the inflammation of the tear, I have used only the thin frozen solid intense ice packs, and again - the numbing, decreased nerve transmission speed, descending inhibitory control, and perhaps decreased catecholamine production? - all combine to let me relax enough to fall asleep.
Sleep with shoulder pain in particular is hard, and something the NIH is encouraging applications for. There are post surgery pillows for shoulders and specific support of different body areas, too, allowing for the overused protective muscles that are often the cause of pain to not be needed (and thus not to wake you up).
Do ice and vibration work for all kinds of pain?
No - ice and vibration work well when the body's nervous system is functioning normally. Injuries, procedures, and muscle pain after surgery or physical therapy respond well. With pain that has gone on a long time, or pain caused by damage to the nerves, direct stimulation will increase pain. With pain from shingles (herpetic neuralgia) or chronic inflammation (fibromyalgia, long COVID, mast cell degeneration) peripheral physiology likely won't help.
What does help for neuropathic pain?
For diabetic neuropathy or other neuropathic damage, the light touch nerve frequencies may help more (like TENS units). New research shows that intentionally damaging misfiring nerves can help for months, as with 8% Capsaicin temporarily frying the TRPV2 receptors on the nerves. CRPS, a regional syndrome with damaged nerves, will likely hurt more with direct nerve stimulation but may be helped by an interrupting nerve stimulation closer to the brain than the region that hurts.
What is Gate Control? Is Vibration the same thing as TENS (transcutaneous electrical nerve stimulation)?
Gate control is the 1965 concept by Melzack and Wall that the mechanoreceptors (nerves that receive touch signals, from light touch to pressure to movement) filter out pain signals in the spine. The idea initially was that triggering these nerves with electricity would "shut the gate" on sharp pain. Instead, different frequencies and depth and amplitude (strength) are required to activate each of the nerves. TENS electricity activates tingly superficial light touch nerves, so it's good to filter out tingly pain like neuropathies. In 2017 it was discovered that motion is most effective in shutting that gate on intense pain; the exact right frequency of vibration can trigger the deep Pacinian nerves that decrease pain.
What is conditioned pain modulation (CPM) or Descending Noxious Inhibitory control (DNIC)? CPM includes ice or unpleasant sensations like pinching. Ice passes sensations of cold to the brain, where the conductor essentially says, “Oh, this sensation is obnoxious, but it’s not dangerous. I will decrease sensations coming from everywhere.” It activates an area called the PAG that inhibits pain. Pinching or self-causing pain in another area is different - it lets the brain know you're in control of the pain, so the knowledge that you can stop it reduces how intensely you're feeling pain.
Dr. Judith Scheman and the Five-finger breathing technique
Five-finger breathing is a simple, powerful breathing technique for deep relaxation and pain relief. Pain specialist and behavioral medicine psychologist Dr. Judith Scheman, Ph.D., explains how to do it in order to relax, unwind and manage pain.
Here is a free workbook of resources you can use to create your own personalized pain management plan, including four sections:
Supplements and Over-the-Counter - Maximizing the effectiveness of short-term ibuprofen, acetaminophen, and sleep aids.Supplements - From magnesium to ginger to boswellia, there are evidence-based supplements that help different kinds of pain.
Physical
In addition to the physiologic and movement options above, sensation interventions can increase beneficial neurotransmitters, and support options can keep the little muscles that cause pain from flaring. Sleep is one of the best ways to escape pain. Being well-rested and well-hydrated makes pain easier to tolerate. Being irritable or slightly dehydrated makes pain worse.
Movement is Medicine
Meditating, yoga, stretching, massage, and exercise block some pain from getting to the brain, and trigger pain relief and inhibition in the brain itself.
A protein in the brain called Brain Derived Neurotrophic Factor improves both thinking and the plasticity to change pain pathways. The strongest way to increase BDNF is exercise, starting at 10 minutes and elevating your heart rate by 20%.
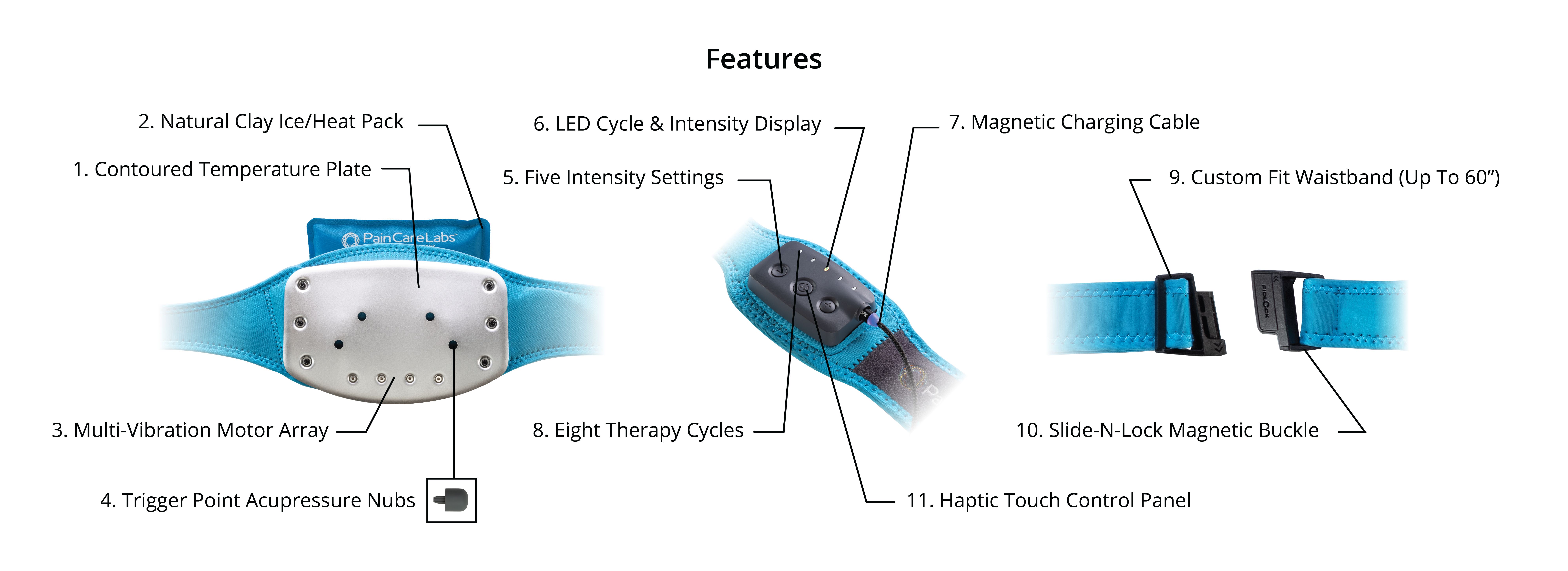
DuoTherm has 1,920 different options, including pressure, heat, cold, and a proprietary harmonic array of mechanical stimulation. DuoTherm is currently in clinical trials to evaluate opioid reduction and to avoid opioid elimination. In a pilot of 20 patients, DuoTherm reduced back pain by 57%, which lasted for 4-5 hours in those who reported duration.